22 July 2020
Frozen Shoulder
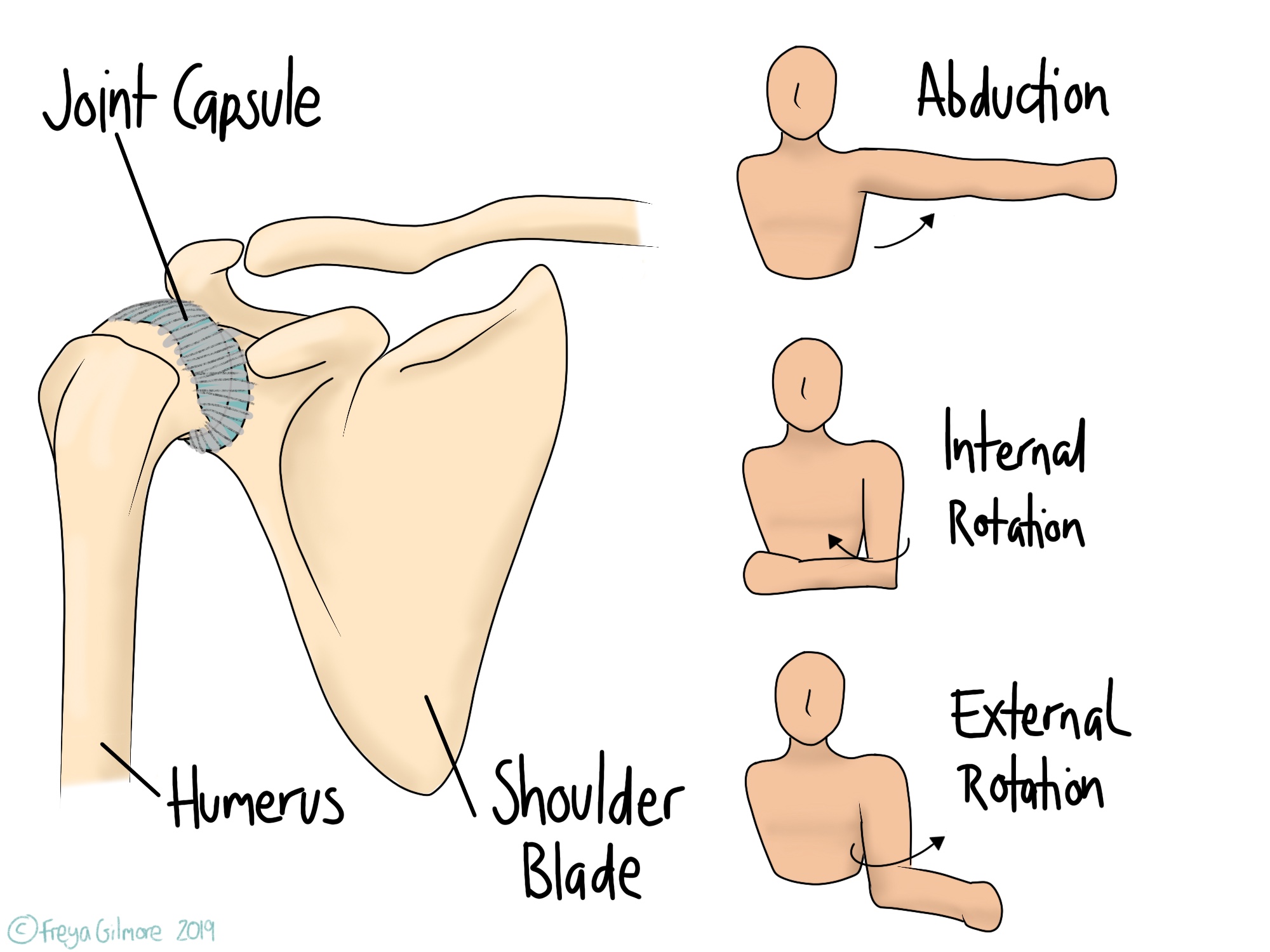
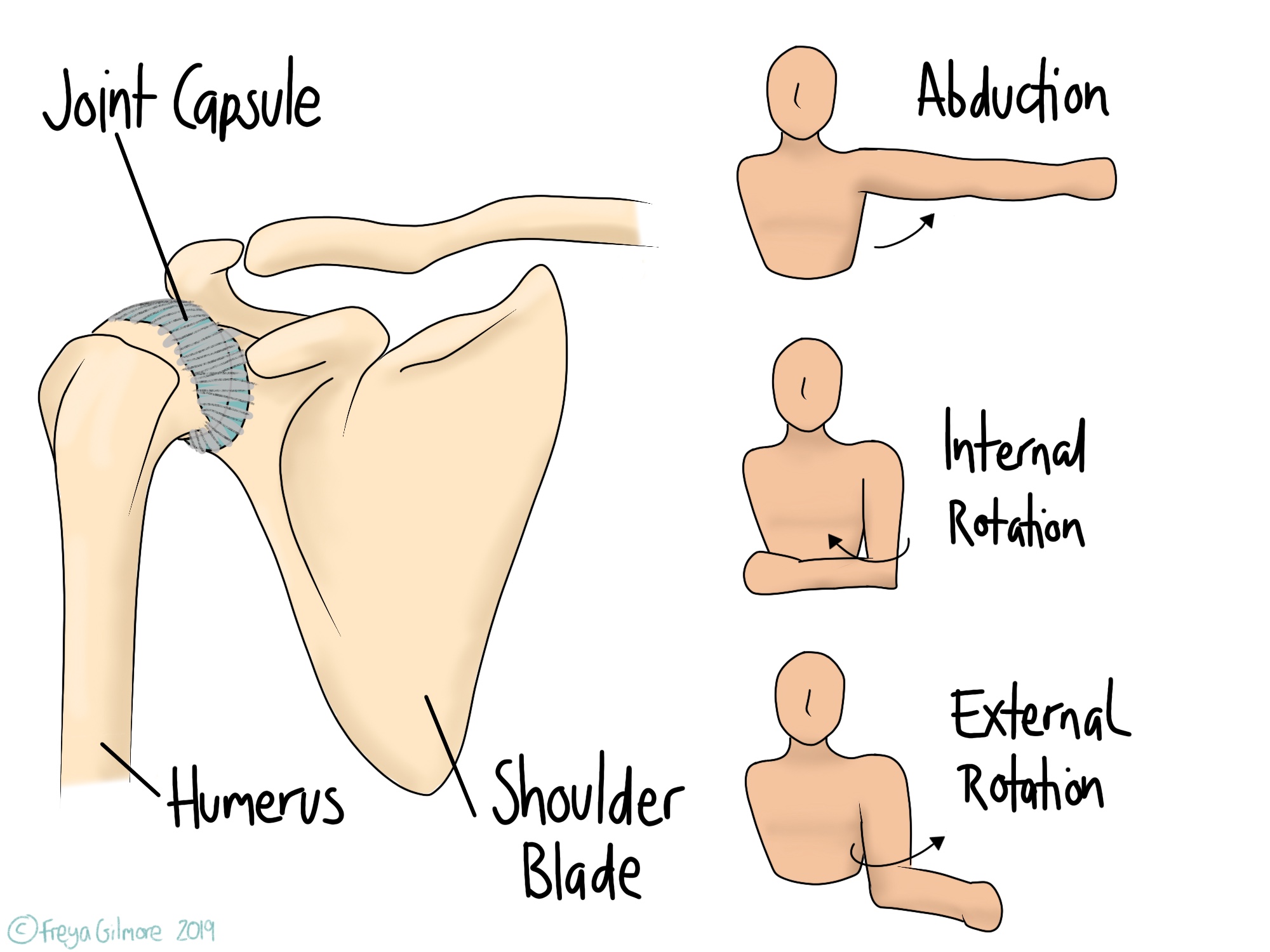
The shoulder is made of a few joints, but in frozen shoulder it is the main ball and socket joint that is affected. This joint is surrounded by a capsule of tissue, which can become inflamed and “sticky”. This is why the official name for frozen shoulder is Adhesive Capsulitis.
An episode can start after trauma or injury, or it can come out of nowhere. Although it is not always clear what has caused an individual’s case, there are some known risk factors.
Diabetes
Risk of developing FSS is around twice as high for a person with diabetes compared to someone without. This is because increased sugar in the blood causes the collagen in the joint capsule to become sticky, as mentioned above.
The risk for other musculoskeletal issues is also higher in people with poorly controlled diabetes.
Shoulder history
Trauma to the shoulder and including immobilisation such as having your arm in a sling can precede frozen shoulder. Surgery around the shoulder has also been linked to onset, although it is unclear whether the surgery itself or the immobilised healing process is the cause.
Having had FSS in one side seems to be a risk factor for developing it later in the other side.
Other diseases
Other conditions have a link with increased risk of FSS:
- Thyroid problems
- Parkinson’s disease
- Some forms of heart disease
Signs and symptoms of Frozen Shoulder
Some movements are particularly affected by FSS: internal and external rotation, and abduction.
- Internal rotation is the movement used when reaching up your back, for example to fasten your bra
- External rotation is the opposite, for example when reaching behind to put your arm in a coat sleeve
- Abduction is bringing your arm out to the side.
From early on in the process, these movements can be sharply painful. This is especially true towards the end of the range of each movement.
The three stage process
The development is defined by three stages:
- Freezing, during which pain intensifies and movement decreases
- Frozen, when pain reduces but movement remains limited
- Thawing, when symptoms begin to resolve
| Stage | Pain | Movement | Duration |
| Freezing | Worsening | Worsening | <9 months |
| Frozen | Improved/plateaued | Most limited | 4-20 months |
| Thawing | Improving | Improving | 5-26 months |
The entire process can take over 4 years, but osteopathy can help to speed it up.
How can osteopathy help with Frozen Shoulder?
Manual therapy such as osteopathy has been shown to improve outcomes for patients with frozen shoulder.
Alongside the changes in the joint itself, the muscles around the shoulder can get very tight during the early stages. Your osteopath can work both the joint and muscles to keep everything as mobile as possible. It can also be helpful to spend time working with the other shoulder to keep it in the best condition in an attempt to avoid a second case of frozen shoulder.
In painful conditions like this, muscles elsewhere can get tight without you realising and cause discomfort elsewhere. One common example is the muscles at the top of the back and into the neck, which tighten up in response to those painful shoulder movements. When these muscles stay tight for long enough, they can cause headaches. Your osteopath can help you prevent this or resolve it if you’re already at that stage.
At Ilminster Osteopathy we specialise in treating disorders of the neck, shoulder, and arm. Book your appointment today.
Learn more
At Ilminster Osteopathy my goal is to help people achieve their goals whatever they may be. Watch our video to find out more.